The AAPPR Annual Conference is a great event every year. It is an opportunity to learn, network and share ideas and this year has proved to be the same.
I had the privilege of presenting alongside LocumTenens.com President Chris Franklin. Our presentation, “The Future of the Healthcare Workforce” took a look at how to create an enduring staffing model. We dove into data about the major industry trends and what that means for staffing. Then, we took a hard look at the options available to hospitals and medical practices and how they can find a sustainable solution. I wanted to take a minute to share some of the key points from our presentation.
At the heart of it, administrators need to think more strategically about optimizing their staffing models. There are three major market factors impacting staffing and outcomes:
Clinician Shortage
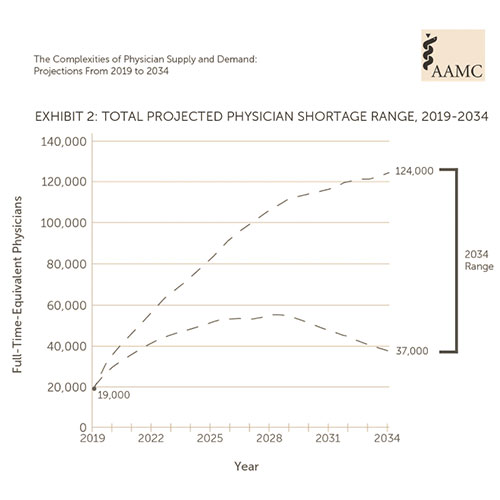
You’ve probably heard this before, but there is a shortage of physicians, and it is projected to become a crisis. By 2034, AAMC projects a deficit of primary care physicians between 17,800 and 48,000. It is equally as sparse for non- primary care specialties with a shortage between 21,000 and 77,100 physicians.
More than 2 of every 5 active physicians in the United States will be 65 or older within the next decade. Demographic forces are the primary driver for this shortage. The situation is serious and the time to adopt new strategies is now.
Burnout
Burnout remains a factor in staffing challenges. According to market research performed by LT.com titled , The Future of Work: Redefining the Role of Physicians in the Gig Economy, 77% of clinicians reported burn out at some level, 40% of clinicians self-reported that they were at least moderately burned out and 17% of respondents said they were “significantly or completely burned out.”
We are starting to see clinicians in their 40s retire, which is concerning since this is the prime of their career and they are choosing to leave medicine. Perhaps economic factors like inflation and a falling stock market, will impact physician practicing rates and bring some clinicians out of retirement, but many have said they will not return to a traditional practice model. This is directly impacting the locums market as well. Providers with less than 10 years of practice experience have more than doubled in the last 3 years. Doctors and Advanced Practice Providers are searching for new and inventive ways to practice and maintain a semblance of work life balance.
Clinical Workforce Gig Thinking
The Great Resignation, the Big Quit, the Grand Reshuffle and the next cleverly named workforce trend will continue to impact healthcare staffing. While we are starting to see the numbers plateau a bit, there is still a tremendous amount of employment mobility.
Physicians are looking for flexibility. They cite high patient loads and long days as their most common dissatisfiers in their jobs. By empowering physicians to own their schedule, administrators may be able to stem the tide of burnout. Additionally, the gig economy has infiltrated healthcare, leaving clinicians with more opportunities outside of traditional roles.
Healthcare is never going to be the same again, but don’t let that scare you. Now is the time to evolve and develop strategies around your healthcare workforce to meet these needs.
So what can we do?
It comes down to innovation and pliability. The global pandemic may have exacerbated physician burnout, but it has also accelerated the growth of flexible staffing models that contribute to higher physician satisfaction and potentially better outcomes for healthcare providers.
Clinicians have a growing preference for agile work models that allow them to control when, where and how they work. On the administration side, addressing these preferences has become a necessity, in order to mitigate the worsening provider shortage.
We believe that the changing preferences of clinicians and the increasing use of contingent labor presents new opportunities for administrators to implement creative staffing models that integrate telehealth and APPs into the existing mold. These options will open hospitals and medical practices to a new pool of practitioners that would otherwise have been inaccessible.
Over the past few years, we’ve learned a great deal when it comes to implementing tele and APP solutions. LT Telehealth is assisting all types of practices and hospital systems to build and launch solutions that utilize telehealth to expand their reach, bring specialty care to those that lack it and construct sustainable programs . We are creating full remote programs as well as hybrid telehealth options that enable facilities to have their providers onsite as well as remote. Successful systems are willing to pilot options and build upon what works. This leads to successful outcomes for both the patients and the provider staff.
Hospitals and practices that invest in a flexible staffing solution have improved access to care and decrease the stress around clinician availability. A fully customized model addresses: service lines, clinician workflows, reimbursements, and patient populations.
We have a history of creating successful, tailor-made programs. If you didn’t get a chance to talk with me at the AAPPR Annual Conference, reach out. We’d love to help you find a sustainable staffing solution.

About the author
Pamela Ograbisz
Vice President of Clinical Operations
Pamela Ograbisz, Associate Vice President of Telehealth for LocumTenens.com. With 20 years of experience in cardiothoracic surgery and internal medicine, she is passionate about delivering quality healthcare in a timely manner. Dr. Ograbisz is confident that telehealth programs are the key to improving health and the overall patient experience.