In a country that prides itself on being a world leader in many respects, this unequal distribution of maternal care has severe consequences, including preventable mortality. Addressing maternal deserts is critical to ensure a safer and healthier future for mothers and infants nationwide. Now more than ever, care for pregnant women in the U.S. is paramount and of the utmost urgency.
But how should this problem be addressed, and who should address it? As the healthcare staffing landscape evolves, clinician workforces – including OB healthcare providers – have been burned out and disincentivized from continuing their traditional roles. A 2023 report by LocumTenens.com shows that Women’s Medicine clinicians have one of the lowest job satisfaction rates of all specialties surveyed. We must make it easier for all frontline maternal care providers to do their jobs with forward-thinking models of care, such as (example).
Understanding Maternal Deserts and the Current State of Access
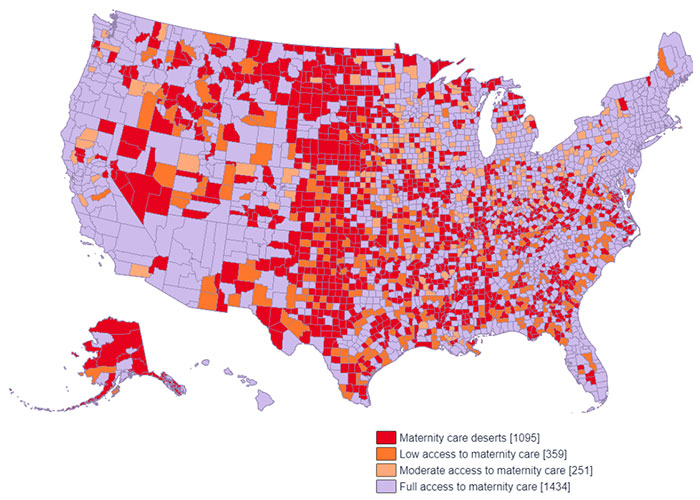
Maternal deserts, as defined by the nonprofit organization March of Dimes, refer to counties lacking hospitals or birth centers offering obstetric care and having no obstetric providers. Between 2020 and 2022, they observed that 247 U.S. counties underwent changes in their maternity care classification, with 94 counties experiencing increased access and 153 witnessing decreased access. This situation calls for immediate intervention to ensure that maternal care is accessible to all pregnant women.
Reasons for the Existence of Maternal Deserts in the U.S.
The existence of maternal deserts can be attributed to various factors, including limited healthcare resources and facilities, particularly in rural areas, where two-thirds of maternal deserts are located.
Sufficient maternal care access has a meaningful effect in communities across the nation. The CDC found that 80% of pregnancy-related deaths in the U.S. are preventable.
Identifying and Mapping Maternal Deserts
Maternal deserts are not confined to specific regions, but rather, they are prevalent across the nation. A comprehensive map detailing the extent of maternal deserts shows that although nearly every state in the country contains counties suffering from the lack of maternal care infrastructures, there is a clear concentration of maternal deserts in the Midwest U.S.
This underscores the urgent need to address this issue on a national scale and improve patient outcomes.
Implementing Solutions to Tackle the Crisis
Addressing maternal deserts requires collaborative efforts at various levels, involving governments, healthcare organizations, and individual clinicians. According to JAMA Network, essential strategies include expanding community-based models that are safe and affordable for low-risk women and addressing workforce challenges in maternal care. Government intervention, as suggested by March of Dimes’ suggested policy solutions, is instrumental in combatting this crisis at a structural level.
According to the National Center for Biotech Information, , healthcare organizations can contribute by adopting multidisciplinary care for women with high-risk comorbidities, addressing structural racism, implementing hospital-wide safety bundles, providing patient education, and promoting regionalized maternal care.
What can Healthcare Organizations and Providers do to Address Maternal Deserts in the U.S.?
Clinicians can make a significant impact by answering the call for travel and locum tenens doctors, thus filling the healthcare provider gap in maternal deserts. In circumstances where a labor shortage exists in healthcare, contingent labor can often help ensure continued coverage while hospitals and clinics continue their search for full-time workforce solutions.
Telehealth solutions also present a viable option to increase access to maternal care in underserved areas. While in-person care will continue to be the backbone of maternal care models, many objectives such as improved patient education can be achieved in telehealth settings.
Conclusion
The existence of maternal deserts in the U.S. demands immediate attention and action. The negative consequences of limited access to maternity care are evident in preventable maternal mortality and adverse outcomes for newborns. By uniting efforts from policymakers, healthcare organizations, and clinicians, we can work towards eliminating maternal deserts and ensuring that every expectant mother has access to high-quality maternal care. Implementing contract-based OB physicians and embracing telehealth solutions are critical steps towards bridging the gap and securing a healthier future for mothers and infants across the country.
References:
1. NPR. (2022). "Millions of Americans are losing access to maternal care. Here's what can be done"
2. Maternity Care Deserts in the U.S., JAMA Network. (2023).
3. Nowhere to Go: Maternity Care Deserts Across the U.S. 2022 Report, March of Dimes. (2022)
4. CDC. "Four in 5 pregnancy-related deaths in the U.S. are preventable."
5. Better Starts For All. "Better Starts for All Pilot Case Study"
6. National Center for Biotech Information. (2019). "Maternal Mortality in the United States: Updates on Trends, Causes, and Solutions"

About the author
Dr. Ashanda Saint Jean
Chair, Obstetrics and Gynecology at Health Alliance Hospitals, a member of WMCHealth
Dr. Ashanda Saint Jean is a graduate of The Sophie Davis School of Biomedical Education/CUNY Medical School. She received her doctorate in medicine from New York Medical College in 1998. She completed her residency training at Danbury Hospital/Yale New-Haven affiliate in Danbury, Connecticut. She is a board- certified OB/GYN Physician with over 20 years of experience working in New York City, focused on the delivery of quality care to underrepresented minority women. Her life’s work has been devoted to the excellence in health care delivery via patient centered comprehensive care, which is inclusive of mental health wellness and combating social determinants of health. Dr. Ashanda Saint Jean is the Chair of Obstetrics and Gynecology at Health Alliance Hospitals of the Hudson Valley, part of the Westchester Medical Center Health Network and an Associate Professor in the Department of OB/GYN at New York Medical College. She is a consultant for the New York City Department of Health, a member of the Ulster County Board of Health, the Hudson Valley section Chair for ACOG District II, the ACOG District II Diversity, Equity and Inclusion delegate for the ACOG national DEI delegation, physician member for the New York State Coalition for Doula Access and an appointed member of both the New York State and New York City Maternal Mortality Review Boards.