Tracking the Growing Need for Geriatric Care
Many factors contribute to life expectancy, and while it is expanding, it brings with it the need for intensive and specialized care for elderly demographics.
- Due to improvements in healthcare, hygiene, lifestyle and other reasons, life expectancy has doubled in the last 200 years.
- During the last century, the growth of life expectancy of the nation’s over-65 population grew five times faster than the overall rate.
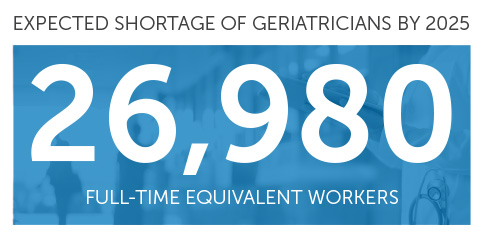
- The US Department of Health and Human Services projects that by 2025, the national shortage of geriatricians will be numbered at 26,980 providers.
The shortage hits different regions and demographics differently, with minorities and rural areas experiencing the deepest gaps between supply and demand. To break out of the traditional thinking that led to this scenario, this shortage will require innovative solutions.
Locum Tenens Workforce Deployment
As the nation’s clinician workforce exits the workforce in greater numbers and in earlier stages in their career, healthcare organizations are increasingly relying on the flexibility of contingent labor solutions to address supply gaps.
- A recent report showed that 71% of contractors and locum tenens clinicians reported little or none of the burnout affecting full-time providers.
- Locum tenens healthcare professionals comprise an eager workforce solution for organizations building new programs, driven by competitive compensation rates and the desire to serve in areas where their expertise is in demand.
Tagging in AGNPs
To bridge this growing gap, healthcare organizations are turning to alternative care models that include Advanced Gerontological Nurse Practitioners (AGNPs). These skilled care providers, while not replacing geriatricians, can play a vital role in delivering necessary and high-quality care to older adults—but have often gone overlooked as a workforce solution due to a historical focus on physicians as well as limited awareness around their scope of practice.
Building a Senior-Focused Primary Care Program
Healthcare facilities do not necessarily need a permanent geriatric doctor on staff full-time. Instead, they can leverage the expertise of locum tenens geriatricians to build and establish a senior-focused primary care program. Here’s how it works:
- A locum geriatrician can be brought in to assess the facility's needs and design a comprehensive program tailored to the specific population it serves.
- This program can be developed over a defined period, such as 3 months or 6 months, and the locum geriatrician can work closely with Hospitalist, EM Physicians, Psychiatrists, Specialists and AGNPs and to ensure seamless delivery of episodic and longitudinal care to the patient while on-site and once the patient returns home.
- By training these clinicians to provide specialized care to older adults, the program becomes sustainable even after the locum tenens physician moves on to their next assignment.
The Growth of Medicare Advantage and its Impact
The rise of Medicare Advantage plans has also added complexity to the landscape of geriatric care. As these plans gain momentum, healthcare facilities must navigate reimbursement structures and adapt their care models to provide cost-effective, value-based care.
Unlocking Revenue with Time-Based Codes
One often overlooked aspect of primary care is the importance of having a billing strategy in order to prevent lost revenue. Properly documenting and billing for time-based codes can significantly impact the financial sustainability of geriatric care programs. By optimizing coding practices, healthcare organizations can ensure they receive appropriate reimbursement for the care they provide.
Although a strategic partner such as LocumTenens.com can expand on the ins and outs of this billing method, some considerations include:
- Outpatient vs. In-patient settings: For outpatient providers, only face-to-face time is counted. For in-patient providers, direct patient contact as well as documentation and consulting are counted.
- Counseling: In time-based billing terms, “counseling” includes test results discussion, diagnostic or treatment recommendations, prognosis, risks and benefits of management options, instructions, education compliance or other risk-factor reduction.
- Eligible providers: While physicians and APPs are eligible for time-based billing, nurses and medical assistants are not.
Enabling Healthcare Organizations to Get Ahead of a Crisis
Through collaboration with a strategic staffing partner that can optimize revenue streams, and embracing innovative care models that provide tangible value to patient communities, healthcare organizations can directly address the rising demand for geriatric care while safeguarding the well-being of our aging population. The time to take proactive measures is now, and innovation will enable healthcare organizations to prevent being dragged along by labor shortage challenges.





