Key takeaways
- With up to 86,000 physicians projected short by 2036, reactive staffing creates burnout cycles and revenue loss
- Manual credentialing delays cost $9,000 daily per provider while centralized systems reduce time-to-start from months to weeks
- Flexibility now outweighs compensation as 41% of satisfied clinicians consider leaving within two years
The trends of 2025 revealed a shift in the industry from crisis management to strategic transformation. However, some practices that worked in the past are actively undermining organizational success in 2026.
1. Treating locum tenens as a last resort
Some medical facilities struggle to leverage contingent staffing solutions as a core strategy and continue to see them as emergency coverage only. This mindset of reactivity reinforces chronic operational problems in an environment where the AAMC projects a shortage of 13,500 to 86,000 physicians by 2036. Rural areas bear the brunt of this, facing a 58% in the coming years versus 5% in urban centers across all specialties. Traditional recruitment timelines on the scale of months don't match the operational realities associated when gaps in coverage are on the line.
Organizations with a strategic view of locum tenens as an infrastructure advantage gain the flexibility to:
- Maintain service continuity
- Scale capacity for seasonal demand and foreseeable personnel outages
- Test new service lines before permanent commitments
- Provide staff with sustainable schedules that reduce burnout
Source: AAMC
2. Treating credentialing as siloed, manual processes
Traditionally, healthcare facilities relied on fragmented workflows managed through spreadsheets and email chains. Each provider required several months (sometimes 90 to 150 days) to get through credentialing, with provider enrollment handled separately.

Research shows organizations lose an average of $9,000 per day when providers cannot practice due to credentialing delays. Disconnected, manual processes lead to gaps in compliance, liability exposure and frustration for providers which negatively impacts candidate acceptance rates.
A modern workforce strategy starts with digital infrastructure that leverages sophisticated automation, enables instant verification, creates more fluid and portable records and reduces time-to-start from months to weeks.
3. Operating without centralized workforce visibility
The daily throughput of healthcare systems encompasses a vast variety of tasks, processes, people and data. Workforce management alone includes managing permanent employees, locum tenens providers, per diem staff and multiple agencies (often through separate systems) in order to provide a competent care offering. Decision-makers regularly lack visibility into meaningful data points around total labor costs or the performance of vendors.
The vendor management system market in particular is projected to grow to $15.2 billion by 2033, with healthcare as the fastest-growing vertical reflecting an urgent operational necessity.
Without centralized visibility, organizations routinely suffer points of inefficiency, such as:
- Overpaying due to lack of rate transparency
- Experience coverage gaps from poor coordination
- Inability to identify cost-saving opportunities
- Compliance blind spots
Unified platforms provide a single source of truth for all staffing channels, real-time visibility into coverage and costs, analytics for strategic planning and vendor accountability, empowering faster and smarter decision-making for healthcare leaders who want a competitive leap forward.
4. Limiting care to traditional in-person models
Despite growing demand among patients and providers, facilities may still approach virtual care as supplemental to face-to-face.
Hybrid models combining virtual and in-person care prove essential for rural communities facing provider shortages. The $50 billion Rural Health Transformation Program, passed into law in July 2025, is encouraging digital health adoption in 2026.
Forward-thinking organizations are building resilient models now that enhance specialty access for underserved communities which are fluid enough to flourish in a dynamic market.
5. Handling routine provider transitions as one-off crises
Organizations cannot afford to treat every departure, retirement or leave of absence as novel and unique and address it by starting over with custom solutions, scrambling for coverage and repeating the cycle.
Outages happen. According to research by Advisory Board and LocumTenens.com from 2025, while most clinicians are satisfied with their jobs, 28% of those who are satisfied are also considering switching jobs in the next two years.
So why are they leaving? The studied showed that non-compensation factors like flexibility and work-life balance increasingly outweigh pay by itself. When asked, 53% of respondents said they preferred a flexible schedule, more than twice the responses that wanted predictability (23%). Regardless of their work satisfaction, clinicians are motivated to find work that offers flexibility.
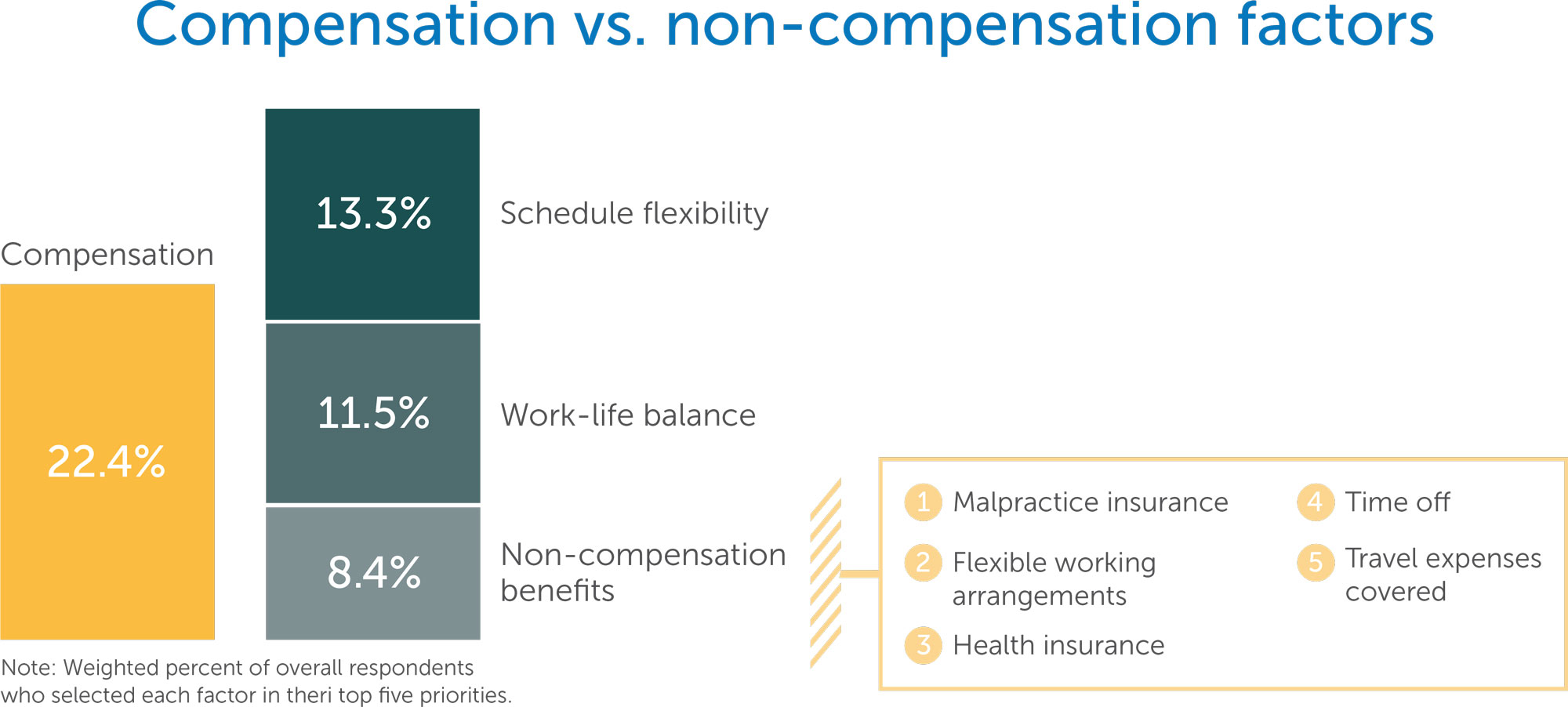
Source: Survey insights: What to know about the clinician workforce today
(Advisory Board and LocumTenens.com, 2025)
Turnover must be planned for even when not specifically anticipated. Maintaining continuity, supporting hand-offs between permanent and temporary staff and enabling knowledge transfer between providers is a process concern and can be planned for with a strategic approach.
From reactive to resilient
Healthcare organizations in 2026 cannot afford to operate from a position of perpetual firefighting. The convergence of workforce shortages, policy developments and care model transformation demands a strategic approach to all aspects of workforce planning rather than reactivity. Organizations making this shift will see a palpable competitive advantage.
Strategic workforce planning is now a partnership that shapes organizational capacity to deliver consistent patient care. Contact the team at LocumTenens.com for an expert evaluation of your organization’s throughput and challenges, and a custom-tailored model to build towards.