How has COVID-19 affected the job outlook for physicians and advanced practitioners?
The COVID-19 pandemic turned the world upside down and one of the industries most affected was, without a doubt, healthcare. LocumTenens.com set out to find what United States physicians and advanced practitioners experienced in 2020 and what the job outlook looks like now as United States citizens continue to become vaccinated. A total of 2,300 clinicians responded and provided insight into how COVID-19 altered employment and salary trends, burnout and time off from practicing.
Here are some of the key findings:
Current and future employment:
- Not all clinicians are back to work. In fact, 14% of physicians and advanced practitioners are still unemployed after being furloughed or laid off last year.
- Clinicians are planning on making a job change soon, with 41% planning to change jobs within the next year.
Patient access to care:
- Almost half of child and adolescent psychiatrists reported an increased workload due to COVID-19, highlighting the detrimental impact of the pandemic on pediatric mental health.
- Most clinicians (63%) have or are planning to take time off from practicing within the next few months. With a growing physician shortage and increased patient visits, the U.S. could be facing a harsh summer and fall with even fewer providers to provide care.
Burnout and stress:
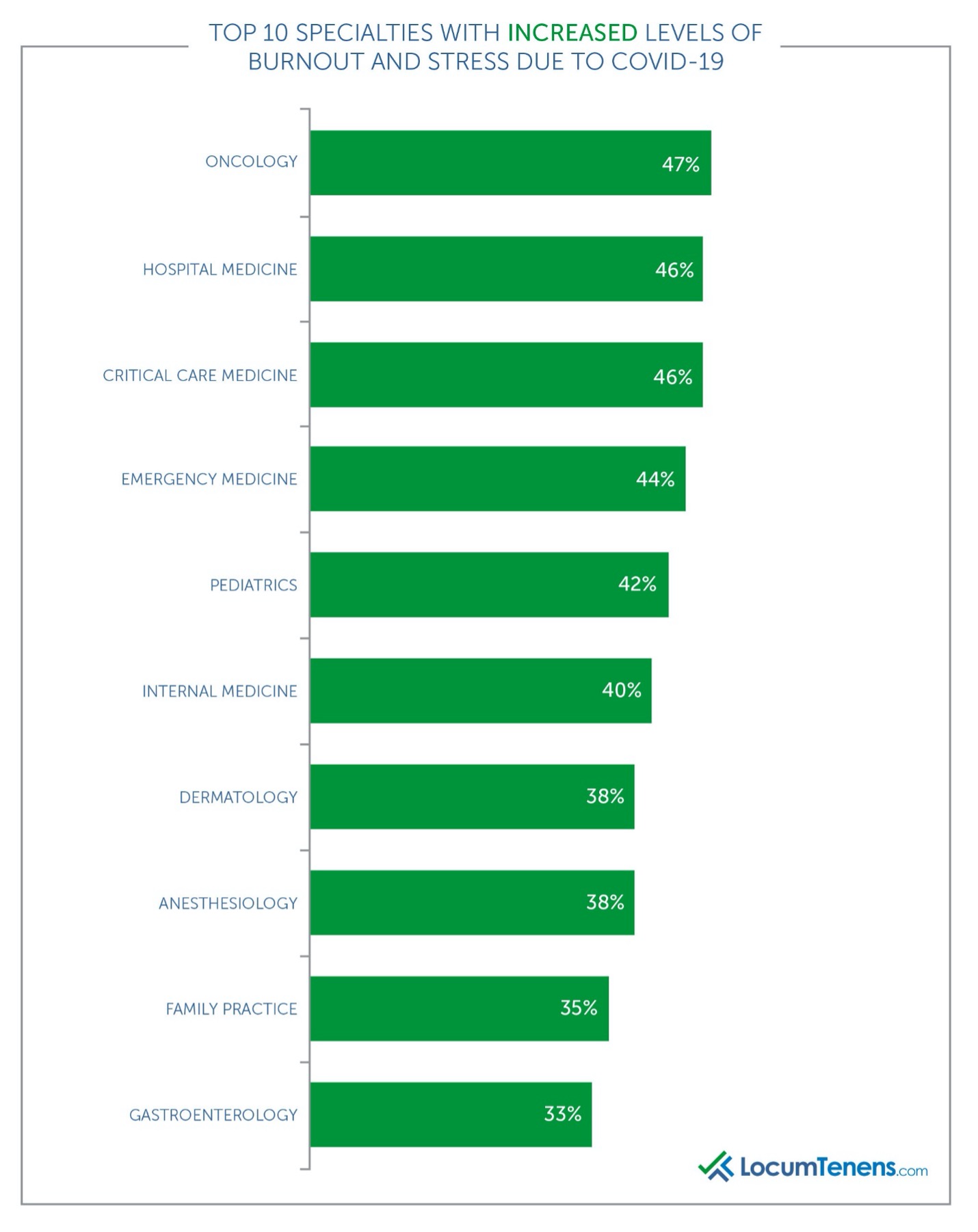
- Overall, 39% of clinicians reported increased levels of stress and burnout due to the pandemic, with the most burned-out specialties being oncology, hospital medicine, critical care medicine and emergency medicine.
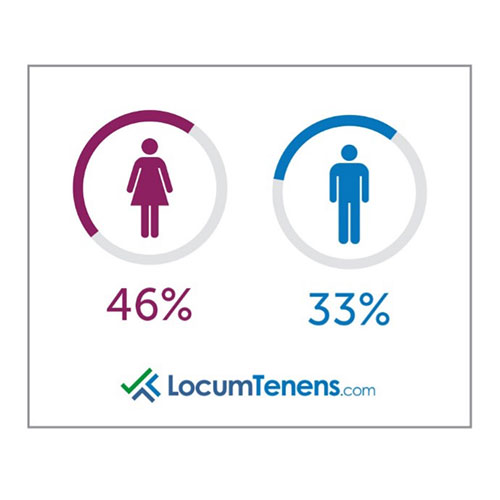
- Millennials reported the highest level of burnout due to COVID-19 at 49%, while 43% of women felt burnout vs. 33% of men.
Employment status after a year of COVID
In June of 2020 we asked clinicians if their organization was affected by furloughs, layoffs or both, and an astounding 54% responded their facility was impacted.
A follow-up survey in September of 2020 found 24% of respondents were professionally affected at some point due to the pandemic. Now that conditions are improving in the U.S. with fewer cases and increased vaccination rates, the healthcare industry is also improving.
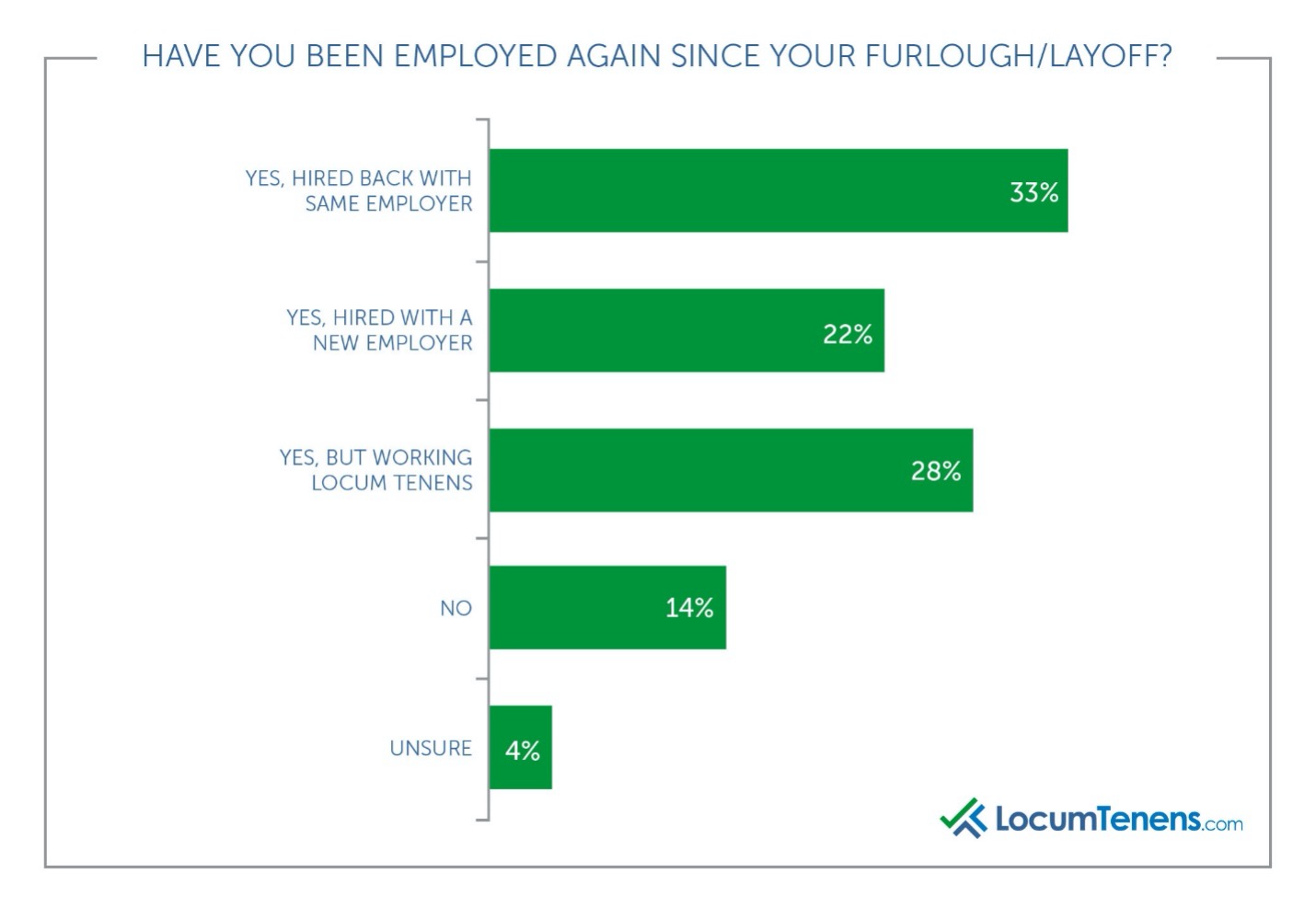
The May 2021 survey shows more than half (55%) of those who lost their jobs are now employed in a full-time position again, and an additional 28% are working locum tenens. In the previous survey from September 2020, 22% stated they had not yet been rehired. That number has now slightly decreased to 14% still unemployed.
When do clinicians plan on making a job change?
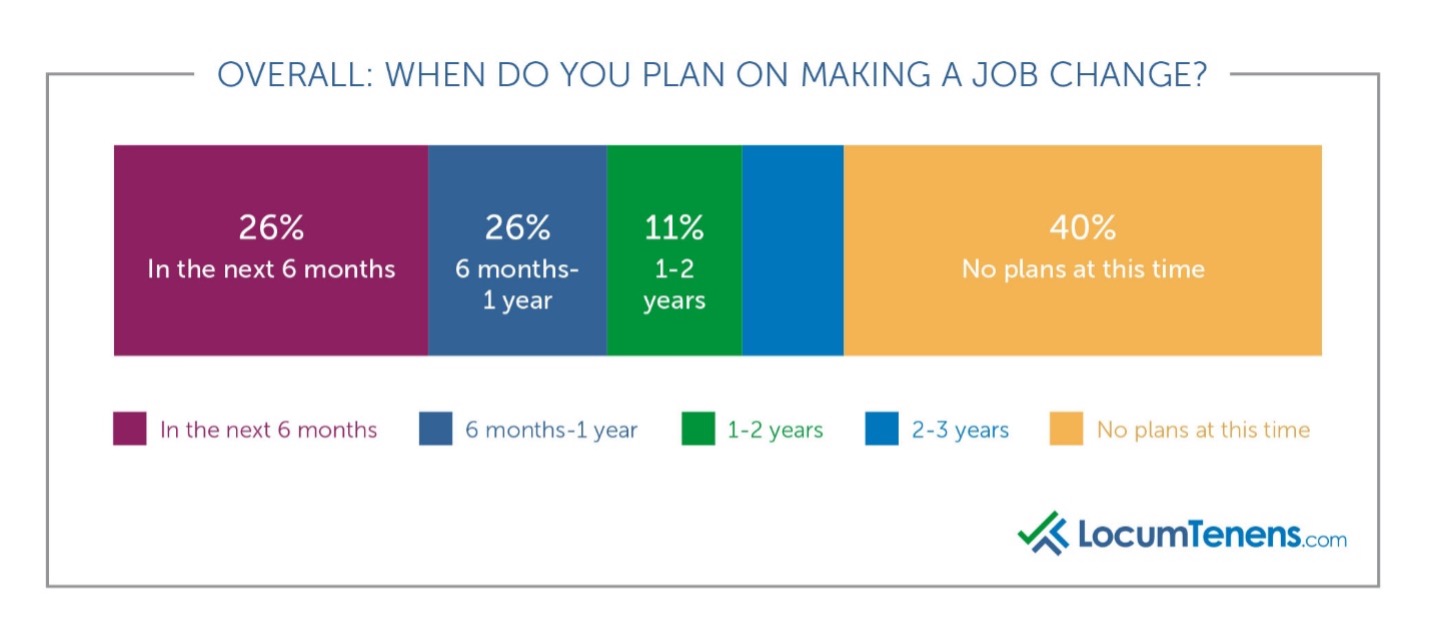
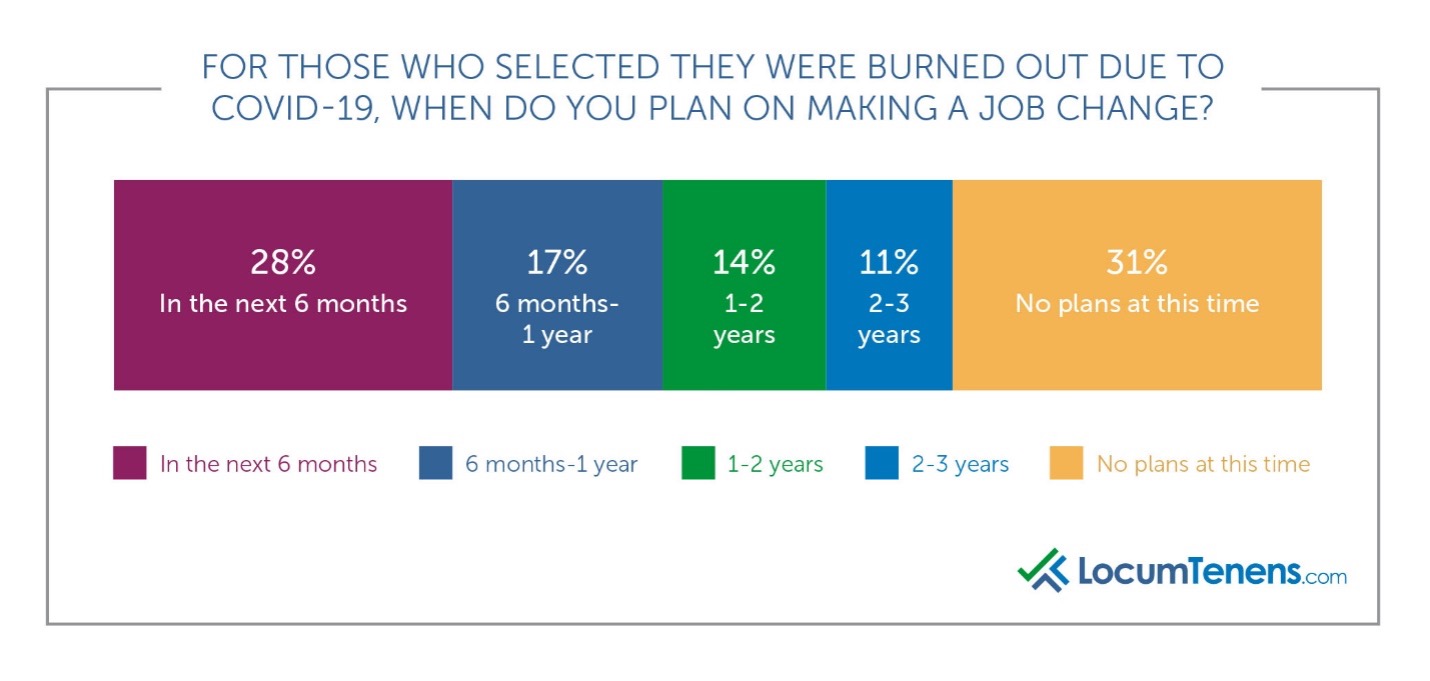
While 40% have no plans to make a job change at this time, 41% are planning to make a job change within the next year, compared to only 36% planning the same in 2019. Of those who are burned out due to COVID-19, that number rises to 45% of healthcare providers planning to change jobs.
Has COVID-19 changed the perception of working locum tenens assignments?
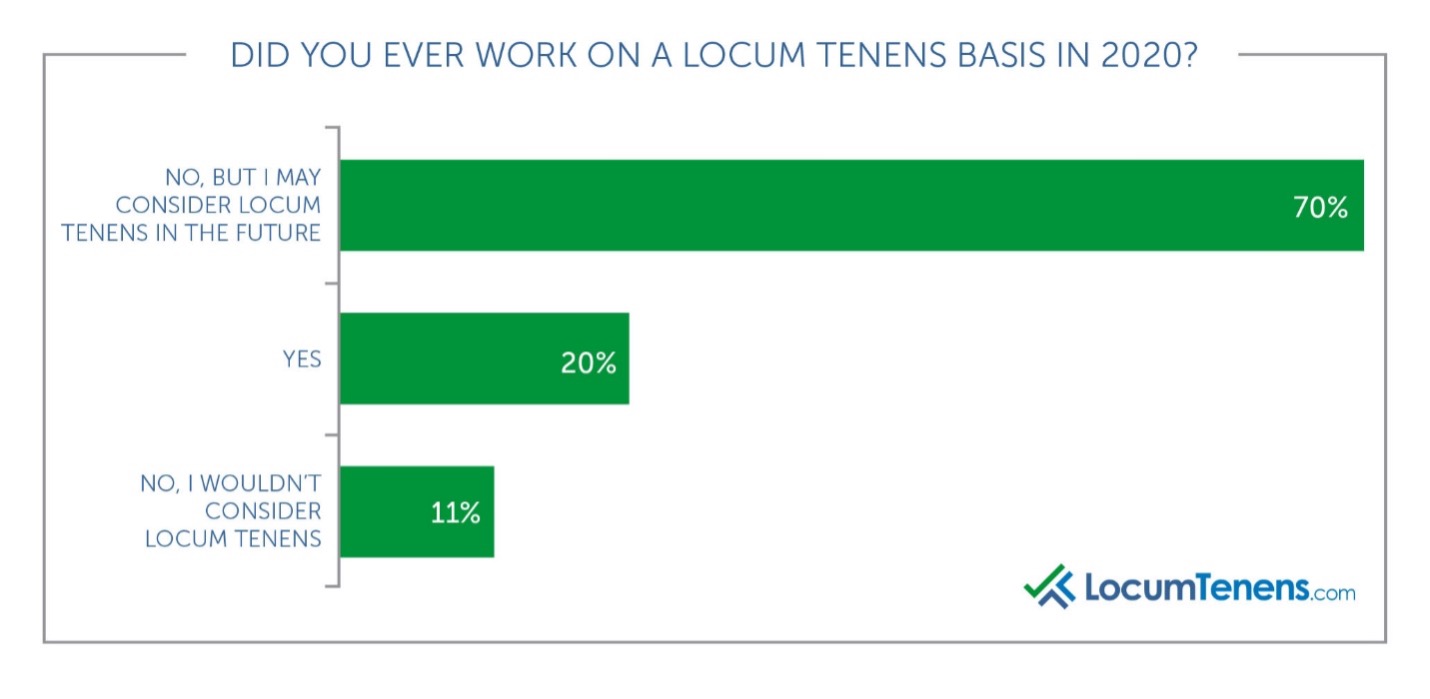
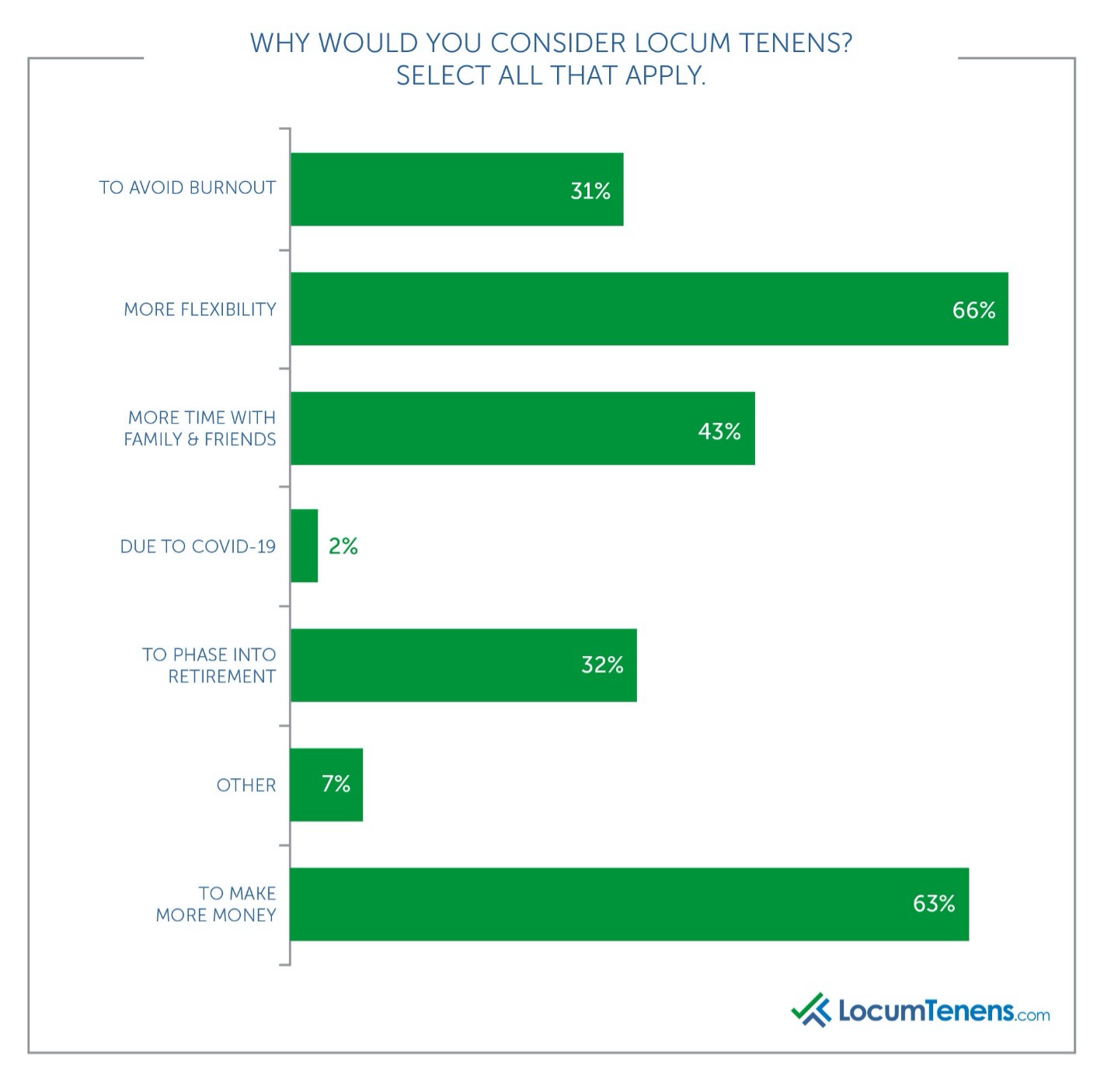
We also asked all respondents if they worked on a locum tenens basis at all during 2020, and while most did not, 70% said they would consider it for the future. Most respondents said they would choose to work locum tenens for more flexibility with the second most popular answer being more money, which is not as surprising after a year of needing to be as flexible as possible.
Salary changes due to COVID-19
Many clinicians said their salary decreased because of COVID-19, with the most common reason due to cut hours or reduced pay, often because of a lack of patients.
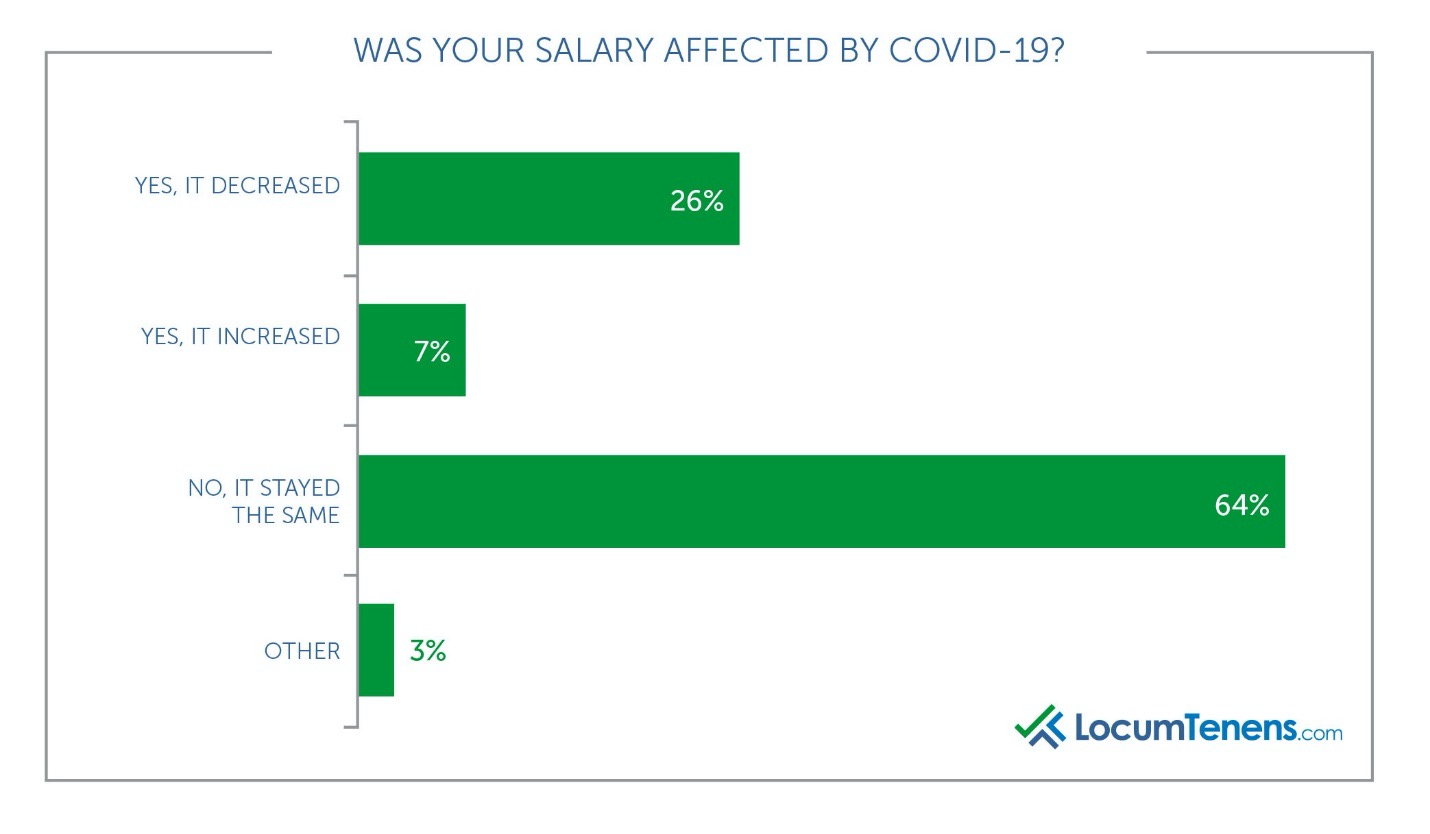
Psychiatrists saw mostly no changes in their salary due to COVID-19, and 7% even reported they received an increase in salary in 2020. Not surprisingly, 20% of critical care physicians also saw an increase in salary due to COVID-19 as their role became even more vital to the influx of hospitalized patients. Similarly, 11% of hospitalists reported increased salary as well.
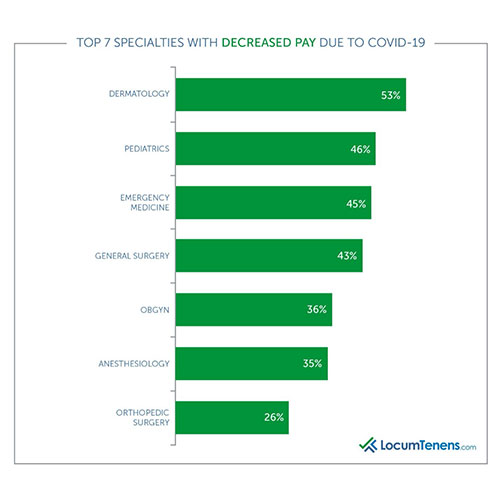
Dermatologists faced the most cuts to their salary due to COVID-19, with more than half (53%) reporting a decrease and only 40% saying their salary remained the same in 2020. A July report from LocumTenens.com found 42% of patients said they would put off their annual dermatology appointments.
The other specialties most negatively affected for pay due to the pandemic were: pediatrics, emergency medicine, general surgery, OBGYN, anesthesiology and orthopedic surgery.
Respondents who reported increase in pay in 2020 attributed it to turning to locum tenens for replacement or supplemental income, receiving hazard pay for those working directly with COVID patients and working more hours.
Physician and advanced practitioner workload in 2020
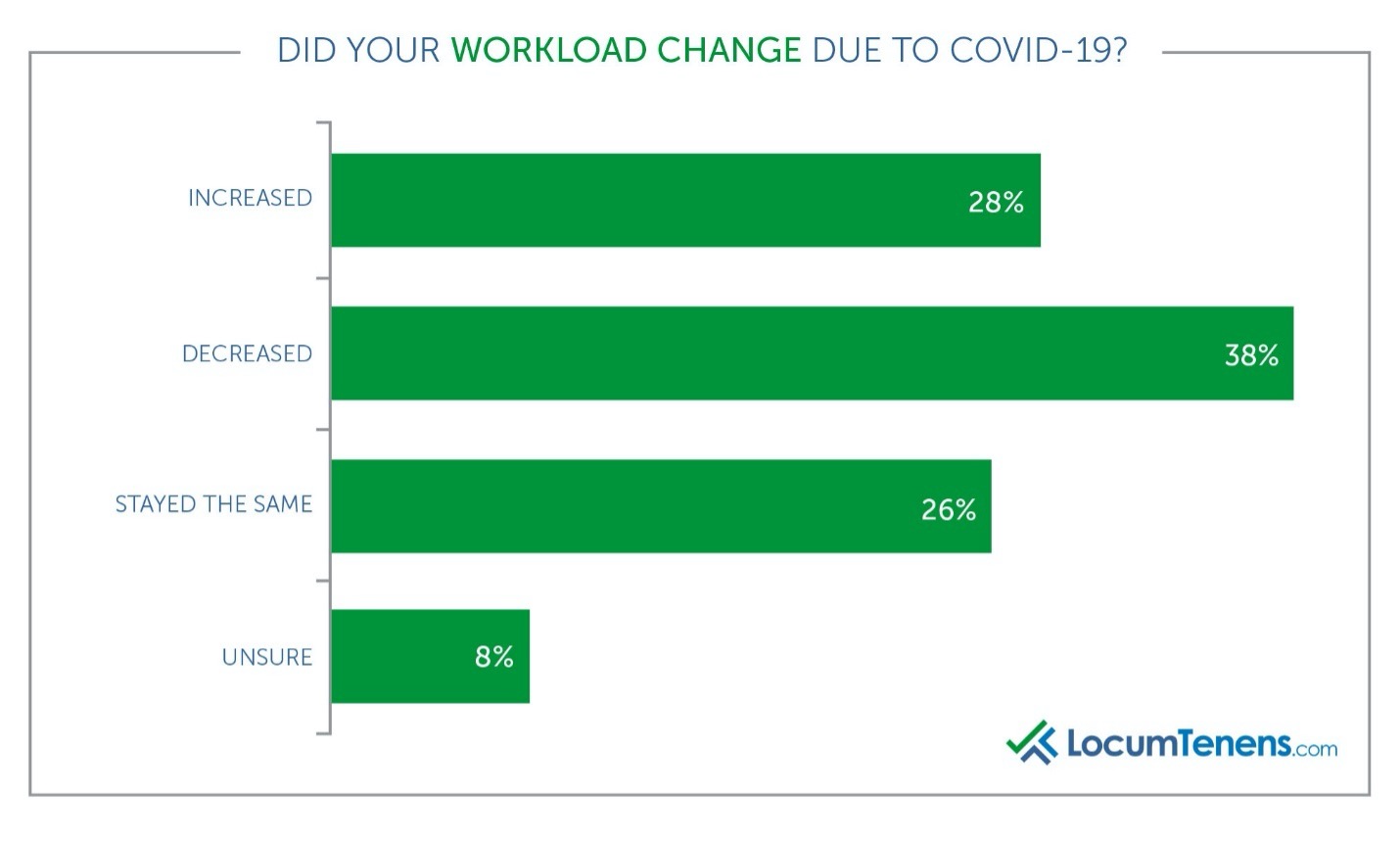
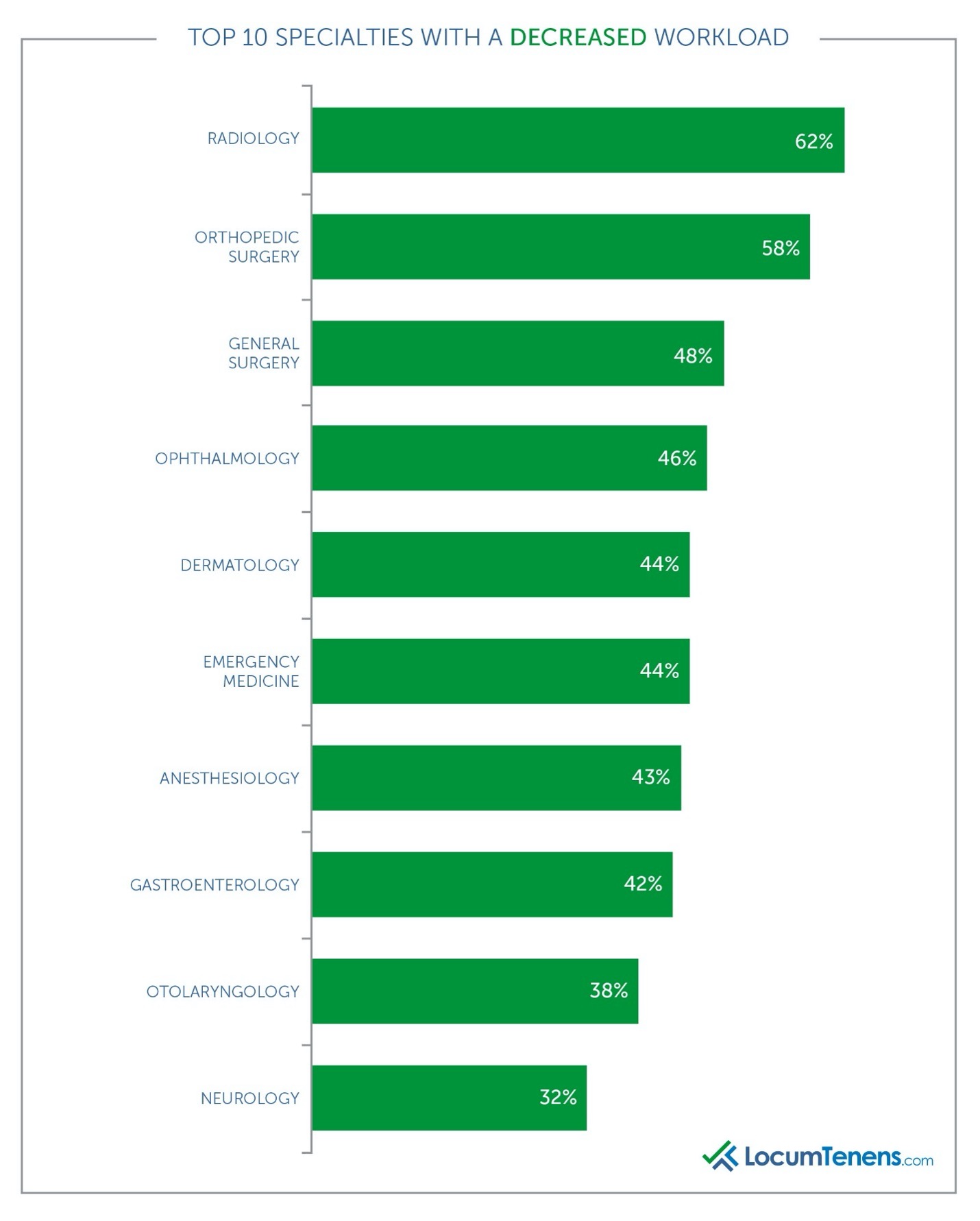
Most clinicians faced unexpected changes to their practice due to COVID-19. Overall, 28% reported an increase to their daily workload, 38% reported a decrease and 26% said their workload stayed the same. Of those who saw a decrease, the vast majority said it was due to the loss in patient volume and the lack of elective surgeries being performed. As one gastroenterologist put it, “we had a significant decrease in outpatient procedures and were only conducting medical emergencies.” A radiologist adds, “Studies were postponed. Screen mammographies were not essential during the initial crisis and our inpatient volume slightly decreased as well.”
Emergency medicine clinicians saw a sharp decline, as one pediatric ED doctor remarked, “we had decreased pediatric ER volumes by approximately 40 percent” and another ED physician assistant said, “there were only two flu cases at my clinic all year; patients were afraid to go to the doctor and our office took a while to get covid tests.”
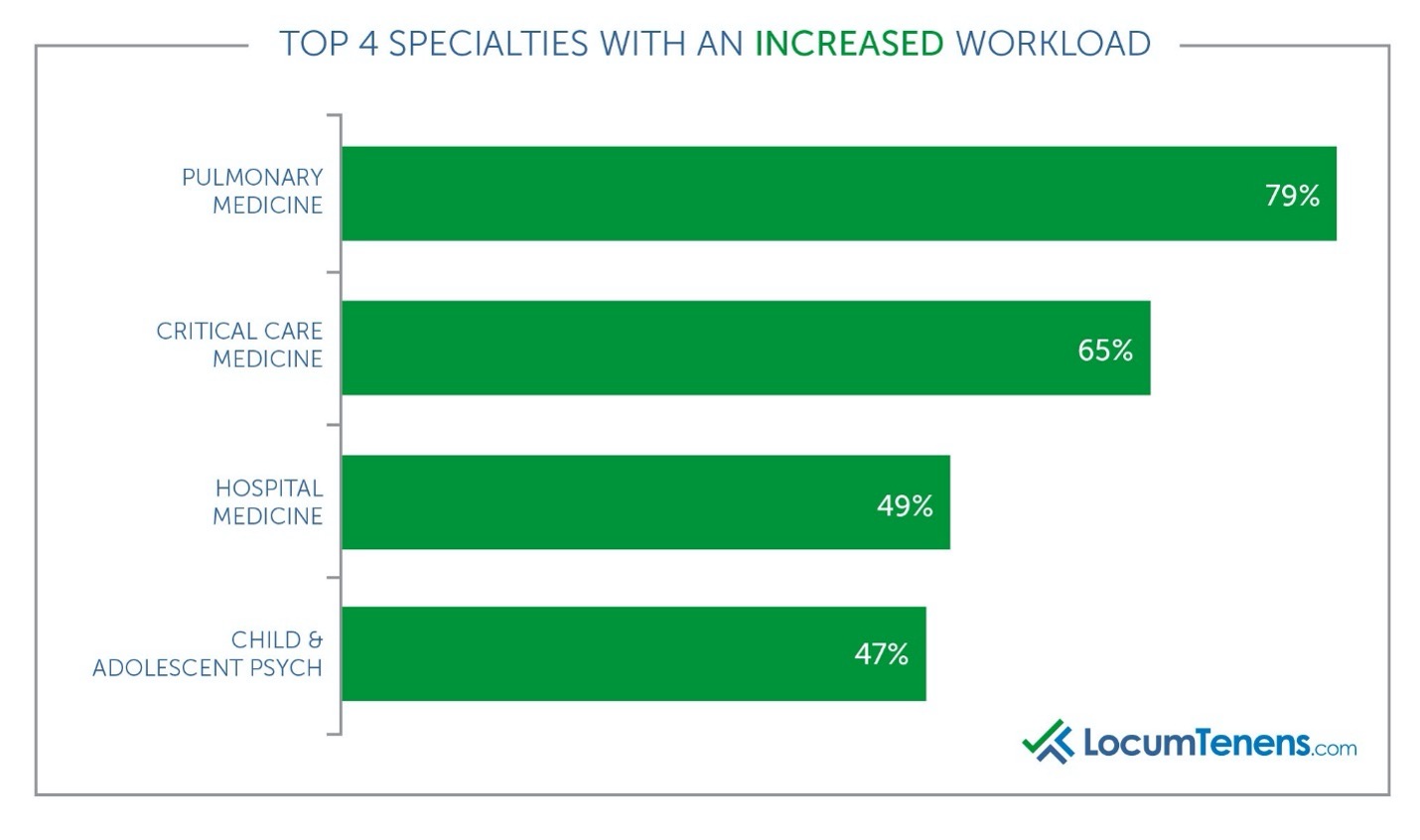
It’s not a surprise that hospitalists and critical care specialists saw an increased workload in 2020. Almost half of hospitalists (49%) reported an increased workload due to COVID-19 and 65% of critical care medicine clinicians reported the same. Pulmonologists were clearly in high demand last year, and 79% of them said they increased their workload.
However, it is interesting to note increased workload in other specialties. A family practitioner stated her employer expected to serve more patient visits but with fewer providers and support staff and the same number of hours required. A neonatal-perinatal medicine physician remarked there was actually “an increased birth rate in my suburban community due to people moving out of NYC.” Many other clinicians commented they had to move out of their regular role into a COVID-specific care ward. Several clinicians commented they saw an increase in patients with COVID with fewer doctors to care for them due to the fear of sacrificing their safety. “I was expected to take on more responsibilities related to COVID issues outside of my specialty of neurology.”
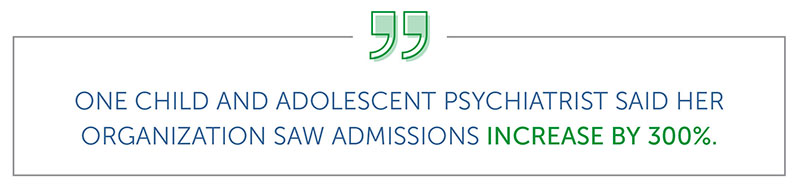
Pediatric and adolescent psychiatrists saw increased workload
The rise of mental health issues during the pandemic is likely to have lasting negative effects as we continue to move forward, and unfortunately, studies are now coming out highlighting how badly children were affected. A recent study by the American Psychiatric Association found more than half of adults with children under 18 in their household say they are concerned about the mental state of their children and almost half say the pandemic has caused mental health problems for one or more of their children.
Mental health facilities across the country are finding an increase in pediatric admissions and suicide attempts. This explains why almost half (47%) of child and adolescent psychiatrists reported an increased workload in 2020 in our survey.
Clinician burnout increased due to COVID-19
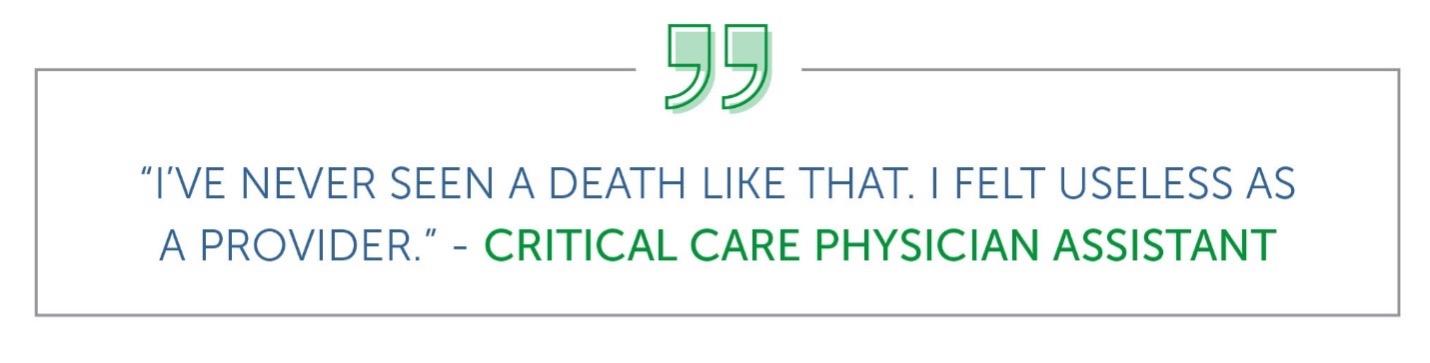
It comes as no surprise many physicians and advanced practitioners (39%) faced increased levels of stress leading to burnout in 2020 due to COVID-19. The specialties with the highest respondents of healthcare providers facing burnout are also not a surprise: hospital medicine, critical care, emergency medicine and pediatrics. These specialties were often at the frontlines battling the coronavirus firsthand around the clock from day one.
Many comments by respondents discussed fear of safety, watching patients suffer or dealing with the mental health of themselves or their patients. “I saw a marked increase in number of patients with mental health crises,” says one pediatric critical care physician. “I had a lot of patients that ended up dying,” adds an ED doctor. Other responses included “putting myself in danger and my children in danger every time I went to work caused me stress” and “seeing near death, increased code blue incidents and the loss of coworkers added to my stress.”
What’s surprising is the other specialties rounding out this list, including hematology/oncology, dermatology, anesthesiology, family practice and gastroenterology. Most respondents for these groups stated their burnout was due to “professional and social isolation,” “working harder with longer hours for decreased compensation” and “higher anxiety and depression overall.” Many respondents stated their facilities were understaffed. Oncologists also added they worried about their immunocompromised patients.
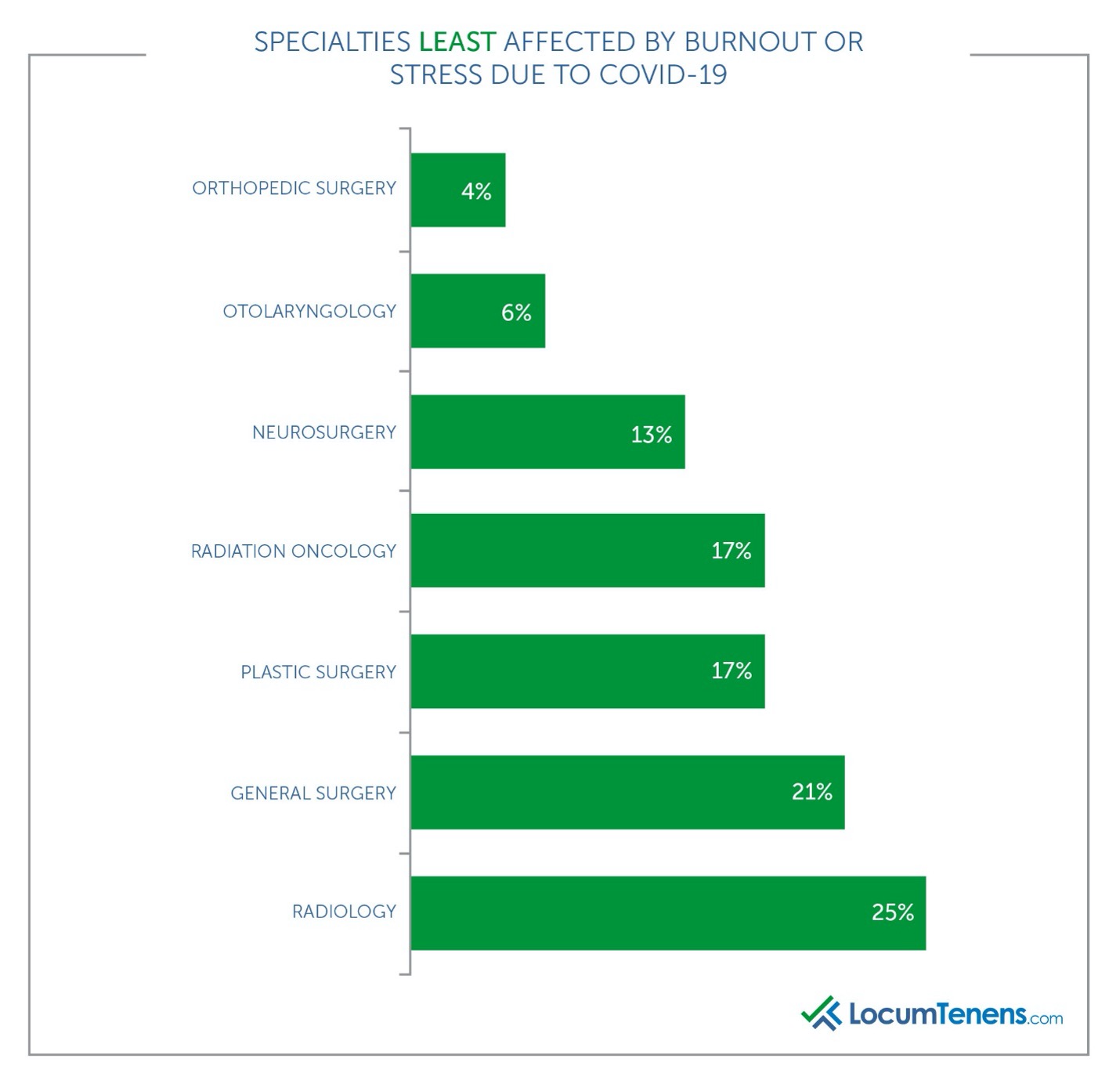
The least affected specialties in terms of burnout due to COVID-19 are radiology, OBGYN and most of the surgical specialties. This could be due to lack of patients and procedures leading to less work to provide. Most of the respondents in these specialties commented that due to the loss of patients, they did not suffer burnout as much as in the past since they were not overworked.
A few of the other specialties were essentially split between being burned out by COVID-19 and not being affected. These included neurology, adult psychiatry and urology. One neurologist commented “the world stopping gave me a chance to re-evaluate my goals and change my lifestyle.” She also mentioned “reinventing” herself and moving into telemedicine.
What about the effects of gender or age gaps on burnout and stress last year?
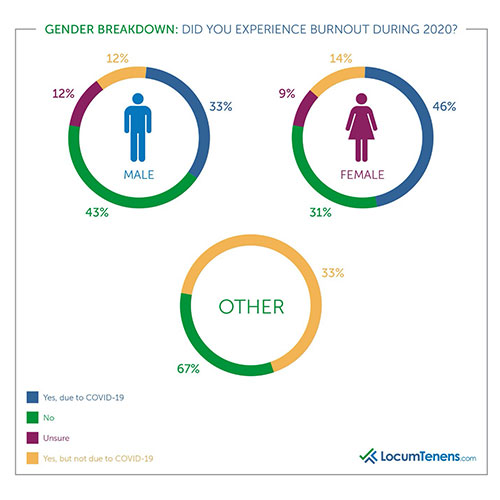
There is a disproportionate effect of those most affected by burnout: 46% of women felt burnout last year due to COVID-19 compared to only 33% of men. In fact, 43% of men said they didn’t feel burnout or stress last year.
Most female respondents reported their burnout was due to the emotional stress of watching patients die, being overworked on COVID floors, worried about family, losing jobs, juggling motherhood and virtual learning with working, and being pregnant. Men who reported stress said it was mostly due to being overworked, dealing with COVID sickness themselves and social isolation.
A female psychiatrist was able to work remotely but commented “I had to split between childcare and working from home; the overall stress and uncertainty added to burnout.” A hospitalist added “juggling kids at home while treating [COVID] patients was stressful.” Another hospitalist struggled to balance being pregnant, treating COVID patients, trying to negotiate maternal leave with her employer and the daily stress of risking her life and her child’s. As many women in the U.S. felt the brunt of COVID on their career, clinicians are no different. One female practitioner stated “I saw fewer patients which meant I made less money. As a single mother, that is very stressful.”
Baby boomers (born between 1946 and 1964) were the least burned out in 2020 due to COVID-19, while millennials (born between 1981 and 1997) had the highest level of burnout due to COVID-19 at 49%, with Generation X respondents (born between 1965 and 1980) close behind at 44%.
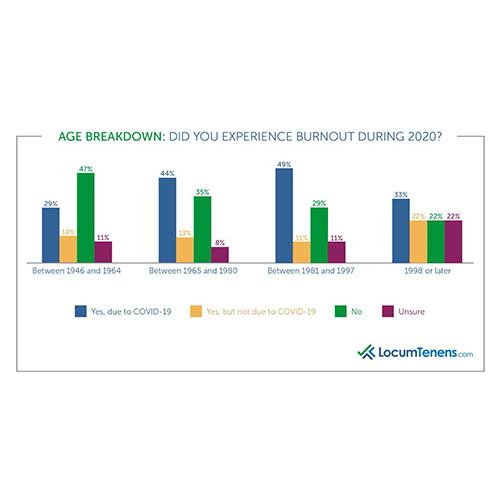
Most millennial clinicians who reported stress and burnout due to COVID-19 stated financial and family stress, as many were providing for small children or worried about keeping them safe. A geriatric NP saw fewer patients but faced more administrative work, was uncertain about keeping her job and worried about a new child at home. Similarly, a young general practitioner stated, “most of my senior colleagues were scared of being infected by covid 19 and were not coming around so workload increased for the junior doctors.” A new emergency medicine physician added “working 10+ days in a row felt exciting at first as a new grad and now feels dreadful.” Physicians who had just finished residency had difficulty finding jobs in specialty fields outside of critical care.
While the millennial clinicians reported higher levels of burnout due to COVID-19, those in Generation X had similar financial worries and many reported they themselves were hospitalized or in constant fear of catching it as they were higher risk.
How are clinicians preparing to recover after burnout?
Now that the U.S. is trending toward relaxing restrictions as more citizens receive COVID-19 vaccinations, many are planning vacations. How many physicians and advanced practitioners have already taken or are planning to take a vacation or time away from work in the next few months?
More than half (63%) of healthcare providers who responded to the survey said they have already or will soon be taking a vacation, with another 10% unsure at the time of the survey. Of those who said they were burned out due to COVID-19, 68% are planning to take time off this summer or fall from practicing medicine.
Are you expecting to take time off from practicing for relaxation or a vacation in the next few months?
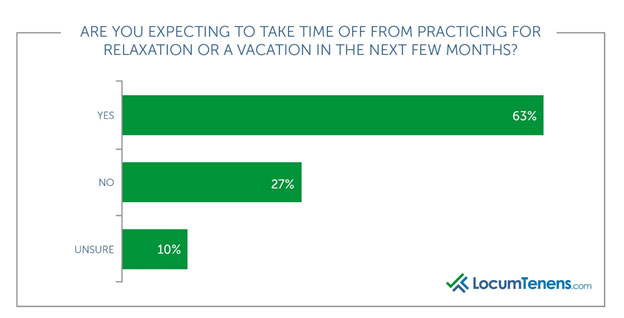
Most respondents said they are taking a much-needed vacation, and in fact, many responded they hadn’t taken a vacation in years but now plan to do so after this stressful year. “Now that I’m vaccinated, I want to travel with my family.”
With 39% of respondents reporting stress after this past year, clinicians from all ages and specialties are reconsidering how or where they practice. “I want to slow down and smell the roses after 29+ years of clinical practice; I want to enjoy my grandchild and travel,” commented a neurologist, while a pediatrician worried about endangering her family through her work says, “I am actually thinking of not practicing medicine anymore.”
Some are deciding to move into mission work on other continents and some respondents are moving into locum tenens work. A family practice nurse practitioner reported, “My employer eliminated paid vacation time during COVID and gave a new contract without PTO and a lower yearly salary. Thus, I did not sign it. I’m now picking up locum positions to allow vacations between assignments.” A psychiatrist added, “I want to take off from work and I want to go back to locums, not employed, so I can go back to travel in places I haven't seen before or go back to places I have been to and loved when I was there.”
Implications for healthcare organizations
With 63% of physicians and advanced practitioners planning to take time off work in the next few months and almost half of respondents looking to find a new job, healthcare organizations will be short-staffed as patients feel more comfortable scheduling their appointments they put off during the pandemic.
There is an expected physician shortage of up to 124,000 by 2034. This will affect patient care when they need it most, especially for those rescheduled preventive medicine and elective procedures. Incorporating locum tenens clinicians into your business strategy could ensure continuity of care, decreasing the likelihood of patients turning elsewhere for available appointments.
Methodology
Invitations for the survey were emailed to a database of more than 220,000 healthcare professionals in May 2021. Some recipients had been placed by LocumTenens.com, and some had not. There was a total of 2300 respondents, both physicians and advanced practitioners, who were self-selected and spanned all 50 states.